An Old-School Solution to a New Epidemic
Featured in Op-Med, a collection of original articles contributed by Doximity members.
“We don’t know what else to do, so we’re calling you,” is what the PA said when she called me to the ER.
“I don’t think anything but a surgery can tell us what is wrong with this patient,” said the ED MD when I got there.
The patient in question was a 53-year-old man whose official weight, recorded in the computer, was 546 pounds and (I’m not making this up) 4.8 ounces — as if that last 4.8 ounces made all the difference. He filled out a bed like bread dough fills a tray. Just lying there, he was dependent on a home BiPAP to assist his breathing. One look at him, and I knew if he went to the OR, it would be a long and risky recovery.
“I woke up and was sitting on the side of the bed and then this horrible pain started,” he told me as he gestured to his whole abdomen with his right hand. “It’s a 100,” he said when I asked him to describe the pain. “I’ve had gallbladder and appendix surgeries, but this is way worse.” “It always hurt, but it gets really bad at times,” he gasped between hits from his BiPAP, “and the morphine doesn’t touch it.”
When I first examined him, he was exquisitely tender all over his abdomen, but not focal. But his belly was soft. The exam was inconsistent, so I went old school and distracted him. I got him talking about how the doctors who had done his cholecystectomy had “screwed it up,” and had had to do an open surgery. While he editorialized, I subtly pressed on his belly and got little response, which reassured me he did not have peritonitis but failed to help me localize the source of the pain.
“Just open me up and cut it out,” he begged.
OK, but cut what out, I thought.
Frustrated by the lack of an answer or even a clear direction to move in, I excused myself from the patient’s room with one of my favorite stall tactics, “I’m going to go look at your X-rays, I’ll be back in a few minutes.”
I reviewed his labs first. They showed a WBC of 13.4 with a left shift and a lactate of 4.3. The rest of his CBC, comprehensive metabolic panel, lipase, and urinalysis were all normal. This seemed to confirm he was sick but gave me little direction. Unable to perform a CT due to the patient’s weight, the ER had gotten plain abdominal films. Those films did not show free air or a concerning bowel gas pattern, but the loss of detail inherent in pushing X-rays through so much tissue limited what I could say with confidence. Perplexed as to what to do next, I took myself on a walk through the deserted back halls of the hospital. The thoughts that ran through my head were uncharitable.
I don’t believe this.
It’s so unfair.
Why do I have to deal with this problem?
It’s not my fault he got himself so damn fat.
… I was right that the patient’s obesity wasn’t my fault, but it was now my problem. I needed to deal with it. I was concerned about a closed-loop small bowel obstruction, injury to the intestines or perforated diverticulitis, and frustrated because a CT scan would give me an answer. If only he weren’t so obese, this would be easier. Without a CT, the only way to diagnose the cause of is abdominal pain seemed to be exploratory surgery. Given his co-morbidities, that was not a decision to be made lightly.
Back in my early days as a surgeon, negative exploratory laparotomies were just a part of doing the job. If a surgeon did not do a negative exploration once in a while, that surgeon was likely leaving pathology behind. But this patient would do very badly with an incision on his belly if he did not need one. I couldn’t afford to be cavalier. As I paced, I thought back to the steps of an exploratory laparotomy from the days before CT, which got me thinking about how we decide whom to operate on. Despite all of the discussion, it often comes down to the instinct of an experienced surgeon. In this case, my instincts were telling me this man did not belong in the OR. If I felt he did, I wouldn’t be agonizing over the decision in the hospital basement.
Yet I wasn’t comfortable not having a diagnosis. Although the surgery was high risk, delaying a needed surgery was probably even riskier. I wondered what I would do if I got him in the OR and didn’t find anything. Then the idea hit me: I might do an on-the-table pyelogram (IVP) to rule out a kidney problem. I wouldn’t need to go to the OR to do it; I could do an IVP before surgery, even on a morbidly obese patient.
I burst into the radiology reading room and asked a recent residency graduate, “Can we do a pyelogram?”
His look said, “Why would anyone want to do that?”
I explained the situation. We both agreed that an ultrasound would be of little value, but a pyelogram might work. When we told the radiology technologist what we wanted to do, the first thing the tech did was reach for a book to refresh her memory on how to do a study that had been relegated to history by the CT scanner.
By the time my phone rang, I had moved on to other patients and problems. It was the radiologist. “I think you were right, looks like something is obstructing that kidney.” Neither of us had seen a stone on the plain films, nor could we see one on the IVP, but the faint and fuzzy shadow of the collecting system on the right was definitely dilated with contrast. It was a diagnosis that fit with the severe, intermittent nature of the patient’s pain. Better yet, it was a diagnosis that did not require me to put an incision on his belly and relegate him to a long, dangerous, and challenging recovery.
I admitted the patient to the hospital floor for pain control, and his symptoms improved as abruptly as they had started. The next morning he was sitting up at the side of the bed and pain-free. I’m not sure which of the two of us was more relieved.
I learned from this experience that we, as doctors, will have patients so obese that they render our usual tools and techniques useless. It may not be our fault, but it is our problem, and we need to learn to deal with it. In this case, I found taking time to walk away from the situation rather than feeling compelled to decide at the bedside gave me some perspective and a chance to think through the problem from a new angle. Going back to diagnostic techniques that were common before CT became the standard made me recognize the other tools I could employ. Ultimately, listening to my instincts made the difference. Although I could have taken this patient to the OR, and I think few doctors would have faulted me for doing so, I just felt it wasn’t right. I followed my instincts, trusted my experience, and ultimately made the right call.
Have you ever needed to use “old” tools to solve new problems? Tell us in the comments!
Charles Black was born and raised among the cornfields of rural Iowa, but moved to the Colorado mountains as soon as he got the chance. He is a general surgeon, writer, photographer, outdoorsman, trail runner, and fires-side philosopher. His musing on medicine and life in general can be found here and you can view his photography here. Dr. Black was a 2019-2020 Doximity Op-Med Fellow and is currently a 2020–2021 Doximity Op-Med Fellow.
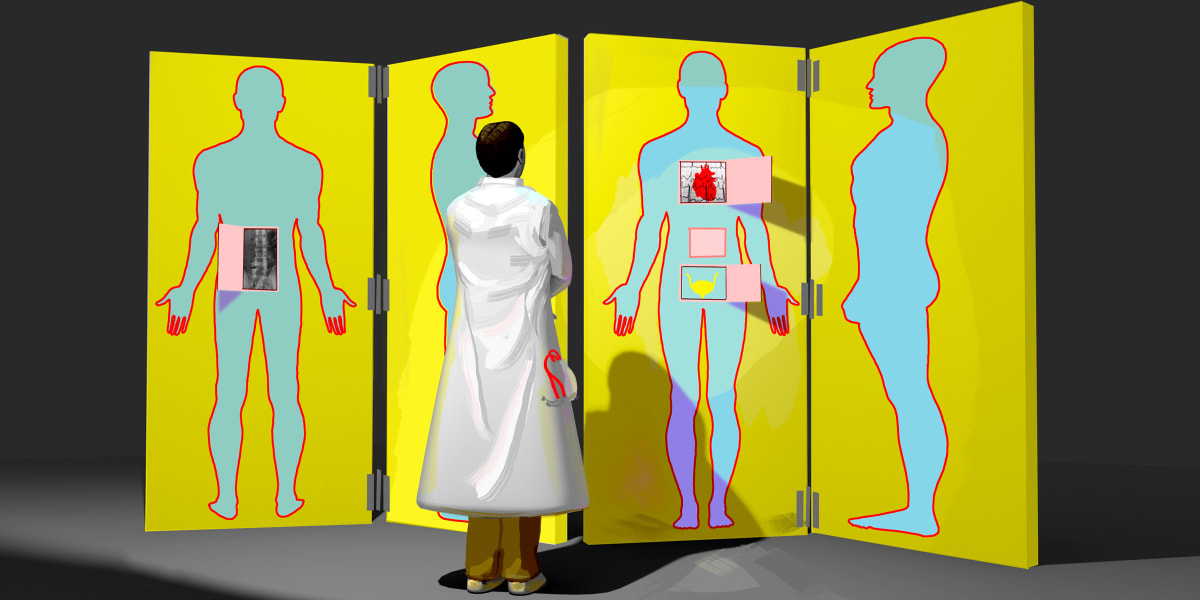
Illustration by Jennifer Bogartz