Many young and healthy Americans assume they are safe because they won’t die from the COVID-19. Death is not the only way it can hurt them.
It is true that only a small percent of people who become infected with COVID-19 die from the virus, but that does not tell the whole story. Many of the survivors are finding life after the virus is not the same. Weeks and even months after testing positive, Americans find that their lives have not returned to normal, and there is no guarantee that they ever will.
The minority of people who die from the virus capture most media attention, but physicians are discovering long-term problems in survivors. The most common complaints are fatigue, shortness of breath, cough, joint pain, and chest pain. These symptoms vary from annoying to limiting enough that suffers are finding it difficult to return to work. However, more serious adverse effects are possible even in young, healthy individuals. And these more severe problems appear to be more common than initially thought. Let’s take a look at the serious risk that can affect people infected with the virus.
- Cardiovascular: inflammation of the heart muscle has been a serious problem in the ICU, where patients infected with COVID-19 are prone to heart failure, arrhythmia, and cardiac death. A recent study published in JAMA Cardiology1 used magnetic resonance imaging (MRI) to study people’s hearts who had “recovered” from COVID-19. The researchers found that 78% of those tested showed cardiac involvement and found ongoing inflammation in 60%. This study had a median follow-up of 71 days, so these patients were on average, still experiencing cardiac injury and loss of function more than two months after “recovering” from the infection.
- If you think this does not apply to you because you are young and healthy, think again. A study of 26 competitive college athletes who tested positive for COVID-19 but did not require hospitalization or even manifest symptoms showed cardiac inflammation in 12 (46%) at up to 53 days after diagnosis.2 How long can this inflammation go on, and what are the long-term ramification for heart function in the future? No one knows. However, other viruses that affect the heart can result in cardiac dysfunction to the point that transplantation is the only option for those patients. Will COVID-19 sufferers find themselves on a transplant waiting list in the future? It is too soon to know, but also a risk that is not worth taking.
- Respiratory: Lung function abnormalities are the most well known acute effect of the Coronavirus, but long-term harm appears to be prevalent as well. A study published in The Lancet looked3 at 55 recovered COVID-19 patients three months after discharge and found that 39 (71%) of them still had symptoms. Not only did they have symptoms three months out, but they also showed persistent dysfunction in their lungs’ ability to absorb oxygen and expel carbon dioxide. At three months, their chest x-rays remained abnormal with findings of interstitial thickening and fibrosis. Will those changes reverse over time, or are they permanent? Again, it is too early to tell, but another good reason to take precautions to protect yourself from being infected.
- Compounded Cardiovascular and Pulmonary Injury: The combination of lung and heart dysfunction could lead to significant disability. My general medical colleges tell me that they see patients several months out from a COVID-19 diagnosis who are still experiencing limitations in their activity that keeps them from returning to work. Previously active and healthy outdoor people are now finding themselves winded after walking up one flight of stairs. Persistent lung and heart dysfunction combined may lead to severe activity limitations for some patients that may never completely resolve. This would result in long-term compromise in their exercise tolerance that could impact their ability to work and maintain a job.
- Blood Clots and Stroke: Through a mechanism that is not yet understood, there is an increased incidence of blood clots and strokes in COVID-19 patients, especially in the young. A review article in The Lancet Neurology reported the risk of thrombotic events, including stroke, to be 6 to 7 times higher in those infected with COVID-19. Organs that have been infarcted include, kidneys, spleen, intestines,4 and heart.5 How long does the risk of infarction and stroke continue after the initial infection? It is not yet clear, but in several of the case studies I reviewed, people had been discharged and then returned to the hospital with their infarction.
- Neurological: Loss of taste and smell are known symptoms of COVID-19. That is because the virus can move from the nose to invade the body via the olfactory nerve. This not only allows the virus access to the body but more concerningly, it enables access to the brain. Anosmia (the loss of taste and smell) may only be the beginning of the havoc this virus can wreak on the nervous system. Hospitals have reported more serious neurological complications, such as encephalitis, seizures, and strokes. While many outpatients have complained of sleep disturbance, major mood swings, memory problems, and impaired concentration collectively referred to as “brain fog.” Many patients continue to complain of these symptoms 2 to 3 months after the illness’s initial onset.6 Only time will tell if these neurological difficulties will resolve or if it will permanently impair some individuals.
- Psychiatric: Patients who have been diagnosed with COVID-19 report depression and anxiety after their infection. Some of this may be a direct result of the viral infection, while others may result from the stigma and isolation of being infected. “No one wants to be around you once they know you have been infected,” one college student told me. “Even a little cough or sneeze and all your friends are making excuses to leave.”
- Renal: Acute kidney injury has occurred in patients infected with Coronavirus. Although not likely a direct effect of the virus, renal failure can occur due to being ill enough to require an ICU stay. Some patients have even required dialysis.
- Dermatologic: There are reports of rashes and hair loss have in COVID-19 positive individuals. Although not life-threatening, the social consequences and loss of self-esteem can have a long-term impact.
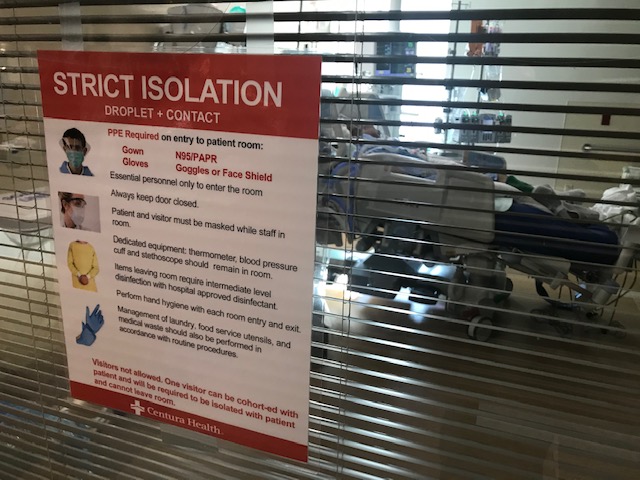
- Even if you don’t get COVID-19, it can still affect you. Hospitals all over the country are being overwhelmed with patients. As ICU’s fill with COVID patients, those beds are not available to care for the patients with other diseases who typically fill the ICU. Due to shortages of physical space and hospital staff, operating rooms are canceling surgeries for other medical problems. People with a non-COVID diagnosis may find it challenging to get the timely care they require. Even without contacting the coronavirus, your health could still suffer as infected patients consume all the medical resources.
Some people seem to believe that it is better to get infected with the virus to develop immunity and move on with their life. I hope the many long-term sequelae listed above have convinced you this may not be a great strategy. Even if you do not require hospitalization, there is no guarantee you may not suffer long-term harm from cardiac and pulmonary dysfunction, blood clots, neurologic impairment or just the social stigma that comes from having been infected with the virus.
Infection with COVID-19 is not as simple as you get a “bad cold,” get over it, and then you are fine. Millions of Americans may face a severe long-term impairment to their physical and mental abilities that could affect their livelihood and quality of life on a possibly permanent basis. It is too soon to know and too serious to risk.
Want to learn more about COVID-19, read this article to learn more about the true danger we as a nation face.
And check out Chuck B Philosophy to learn more about how to be more than just not sick. Learn how to thrive.
1
2 https://jamanetwork.com/journals/jamacardiology/fullarticle/2770645
3 https://www.thelancet.com/journals/eclinm/article/PIIS2589-5370(20)30207-8/fulltext
4 https://wwwnc.cdc.gov/eid/article/26/8/20-1161_article
5 https://www.ahajournals.org/doi/10.1161/CIRCULATIONAHA.120.050809
6 https://jamanetwork.com/journals/jamaneurology/fullarticle/2766766